AHUS (Atypical Hemolytic Uremic Syndrome) is a rare and serious disease that affects the blood and kidneys, often leading to organ damage.
The Basics of AHUS Disease
Atypical Hemolytic Uremic Syndrome, or AHUS disease, is an uncommon but serious condition that primarily impacts the kidneys. It occurs when there is abnormal damage to the blood vessels, particularly in the kidneys, leading to the destruction of red blood cells (hemolysis), low platelet count (thrombocytopenia), and kidney failure. This disease is part of a larger group of conditions known as hemolytic uremic syndrome (HUS), with AHUS being distinguished from the more common form (diarrhea-associated HUS) by its underlying cause and presentation.
AHUS is a complex condition that can often be mistaken for other diseases due to its overlapping symptoms, which makes it challenging to diagnose. It can affect anyone, although it is more commonly diagnosed in children, and if left untreated, it can lead to severe kidney damage, long-term health problems, or even death. The disease is associated with abnormalities in the complement system, a part of the immune system that helps regulate inflammation and protect against infections.
In this article, we will explore what AHUS disease is, how it develops, what causes it, and how it is diagnosed and treated.
What Happens in AHUS?
In AHUS, the immune system plays a crucial role in the pathogenesis of the disease. The immune system’s complement system, which normally helps the body fight infections, is overactive. This overactivity causes damage to the blood vessels, particularly those in the kidneys. As a result, small blood clots form in the blood vessels, leading to a reduction in blood flow, particularly to the kidneys, and causing organ damage.
This condition can cause a range of problems, including:
- Hemolysis: The destruction of red blood cells, which leads to anemia.
- Thrombocytopenia: A low platelet count, which increases the risk of bleeding.
- Kidney Dysfunction: Damage to the kidneys can lead to acute kidney failure and, if untreated, can result in chronic kidney disease.
It’s essential to understand that AHUS is not caused by an infection, as is the case with diarrhea-associated HUS, but instead by genetic mutations or other factors that lead to the overactivation of the complement system. This makes AHUS an autoimmune disease in which the body mistakenly attacks its own tissues.
The Causes and Risk Factors for AHUS
1. Genetic Mutations and Inherited Risk
A significant portion of AHUS cases is associated with genetic mutations. Mutations in certain genes can cause abnormal function of the complement system, leading to its overactivation. The complement system consists of proteins that normally work to help clear infections and remove damaged cells, but in AHUS, the mutations cause it to be hyperactive, damaging the blood vessels and organs in the body.
These mutations are often inherited, and familial AHUS runs in families. The most commonly affected genes are those related to the complement regulatory proteins, such as CFH (complement factor H), CD46, C3, and CFI (complement factor I). Individuals with mutations in these genes may have a higher risk of developing AHUS, although the disease can also occur in individuals without any family history.
2. Environmental Triggers
While AHUS is primarily a genetic disorder, environmental factors can also play a role in triggering the disease, particularly in individuals with a genetic predisposition. Infections, particularly bacterial infections like Escherichia coli (E. coli), can trigger the onset of AHUS. Infections can cause damage to the kidneys, which, combined with an underlying genetic mutation, can lead to the development of AHUS.
Other factors that may trigger the disease include:
- Pregnancy: Pregnancy-related complications, such as pre-eclampsia, can trigger AHUS in individuals who are genetically predisposed.
- Medications: Certain medications, such as immunosuppressive drugs, can lead to an exacerbation of AHUS in susceptible individuals.
- Other autoimmune conditions: Conditions like systemic lupus erythematosus (SLE) may increase the likelihood of developing AHUS.
3. Complement System Dysfunction
As mentioned earlier, AHUS is primarily caused by dysfunction in the complement system, a part of the immune system that helps fight infections. The complement system comprises a series of proteins that are activated to help the immune system fight pathogens. In AHUS, the complement system becomes overactivated, leading to damage to the blood vessels and organs, especially the kidneys.
This overactivity is often triggered by the aforementioned genetic mutations, but it can also be influenced by infections or other environmental triggers.
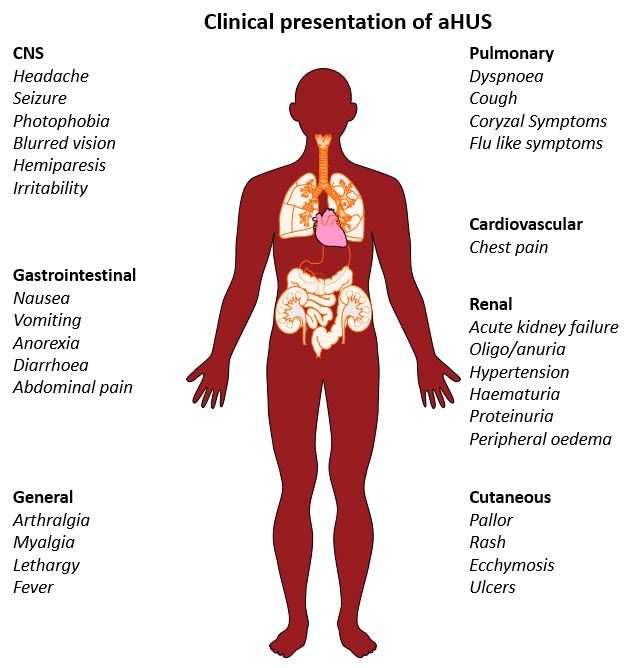
Symptoms of AHUS Disease
The symptoms of AHUS can vary depending on the severity of the disease and which organs are affected. However, common symptoms of AHUS include:
- Fatigue: Due to anemia caused by the destruction of red blood cells.
- Paleness: Often a result of anemia.
- Swelling (Edema): Especially in the legs, ankles, and face, due to kidney damage and fluid retention.
- Decreased Urine Output: Kidney dysfunction can lead to less frequent urination or complete kidney failure.
- Abdominal Pain: This may occur due to inflammation or reduced blood flow to the organs.
- High Blood Pressure (Hypertension): Elevated blood pressure can result from kidney damage or fluid retention.
- Bruising or Bleeding: Thrombocytopenia can lead to easy bruising or spontaneous bleeding, such as nosebleeds or gums bleeding.
The severity of these symptoms can vary, and in some cases, the disease progresses rapidly, leading to acute kidney failure and requiring immediate treatment.
Diagnosis of AHUS
Diagnosing AHUS can be a challenge due to its rare nature and the overlap of symptoms with other kidney diseases. The diagnosis typically involves:
1. Blood Tests
Blood tests are crucial for diagnosing AHUS, particularly to measure:
- Hemoglobin levels: To detect anemia caused by hemolysis.
- Platelet count: To check for thrombocytopenia.
- Creatinine and urea levels: Elevated levels can indicate kidney dysfunction.
- Complement levels: A decrease in certain complement proteins (such as factor H and factor I) can suggest AHUS.
2. Genetic Testing
Genetic testing is often performed to identify mutations in the genes related to the complement system. These mutations can confirm a diagnosis of familial AHUS or genetic predisposition to the disease.
3. Kidney Biopsy
A kidney biopsy may be performed to assess the extent of kidney damage. This can help distinguish AHUS from other forms of kidney disease and guide treatment decisions.
4. Urine Tests
Urine tests can also be used to check for the presence of protein or blood in the urine, which may indicate kidney damage.
Treatment of AHUS
Treatment for AHUS is aimed at controlling the underlying immune system dysfunction and managing the complications of the disease. The specific treatment plan will depend on the severity of the disease, the patient’s age, and the presence of any genetic mutations.
1. Plasma Exchange (Plasmapheresis)
In some cases, plasma exchange (or plasmapheresis) is used to remove the harmful complement proteins and antibodies from the bloodstream. This process can help reduce the overactivation of the immune system and prevent further damage to the kidneys and other organs.
2. Complement Inhibition Therapy
A newer treatment option involves the use of complement inhibitors, such as eculizumab, which specifically targets and blocks the overactive complement system. These medications have been shown to be effective in treating AHUS by preventing further damage to the kidneys and other organs.
3. Kidney Transplant
In severe cases where kidney damage is irreversible, a kidney transplant may be necessary. However, individuals with AHUS may be at higher risk of transplant rejection due to the ongoing complement system dysfunction. Therefore, careful monitoring and complement inhibition therapy are often required after a kidney transplant.
4. Dialysis
For patients with acute kidney failure, dialysis may be necessary to help filter waste products from the blood until kidney function improves.
5. Supportive Care
In addition to specific treatments, patients with AHUS may require supportive care, such as blood transfusions, medication to manage blood pressure, and treatments for anemia or electrolyte imbalances.
Prognosis of AHUS
The prognosis for individuals with AHUS depends on several factors, including how quickly the disease is diagnosed and treated, the severity of kidney damage, and whether the person has any genetic mutations. With early diagnosis and appropriate treatment, many individuals can recover kidney function and lead relatively normal lives. However, without treatment, AHUS can result in permanent kidney damage or kidney failure, which may require long-term dialysis or a kidney transplant.
Key Takeaways: AHUS Disease
➤ AHUS Overview: A rare condition affecting blood and kidneys, leading to damage.
➤ Immune System Role: Overactive complement system causes blood vessel damage.
➤ Genetic Factors: Mutations in genes increase the risk of developing AHUS.
➤ Diverse Symptoms: Common signs include fatigue, swelling, and decreased urine output.
➤ Treatment Options: Plasma exchange and complement inhibitors are key therapies.
➤ Treatment Options: Plasma exchange and complement inhibitors are key therapies.
Frequently Asked Questions: AHUS Disease
What is the primary cause of AHUS disease?
Atypical Hemolytic Uremic Syndrome (AHUS) is primarily caused by genetic mutations that affect the complement system, which is a part of the immune response. These mutations lead to an overactive complement system that damages blood vessels, particularly in the kidneys. This dysfunction can result in hemolysis, thrombocytopenia, and kidney failure.
The most commonly affected genes include CFH (complement factor H), CD46, and C3. Individuals with these mutations may experience a heightened risk of developing AHUS. Additionally, environmental triggers such as infections can exacerbate the condition in genetically predisposed individuals.
How does AHUS disease affect kidney function?
In AHUS disease, the overactivation of the complement system leads to damage in the blood vessels of the kidneys. This damage results in reduced blood flow and can cause acute kidney injury or chronic kidney disease over time.
The condition causes small blood clots to form, which further impairs kidney function. Symptoms may include decreased urine output, swelling due to fluid retention, and elevated blood pressure. If left untreated, AHUS can lead to irreversible kidney damage requiring interventions such as dialysis or transplantation.
What are the common symptoms associated with AHUS disease?
The symptoms of AHUS disease can vary widely among individuals, but common signs include fatigue due to anemia from hemolysis, swelling (edema) from fluid retention, and decreased urine output because of kidney dysfunction.
Other symptoms may include abdominal pain, high blood pressure, and easy bruising or bleeding due to low platelet counts. The severity of these symptoms can escalate rapidly; thus, early recognition and treatment are crucial for better outcomes.
How is AHUS diagnosed?
Diagnosing AHUS disease involves a combination of clinical evaluation and laboratory tests. Blood tests are essential for measuring hemoglobin levels, platelet counts, and creatinine levels to assess kidney function.
Genetic testing may also be performed to identify mutations related to the complement system. In some cases, a kidney biopsy is necessary to evaluate the extent of damage and distinguish AHUS from other renal conditions. Urine tests can help detect protein or blood presence indicative of kidney injury.
What treatment options are available for AHUS disease?
Treatment for Atypical Hemolytic Uremic Syndrome (AHUS) focuses on managing symptoms and addressing underlying immune dysfunction. One common approach is plasma exchange (plasmapheresis), which removes harmful proteins from the bloodstream.
Additionally, complement inhibition therapy using medications like eculizumab has shown promise in halting disease progression. In severe cases where kidney function is irreversibly compromised, a kidney transplant might be necessary. Supportive care such as managing blood pressure and treating anemia also plays a crucial role in comprehensive patient management.
Are there any long-term effects associated with AHUS disease?
The long-term effects of AHUS disease largely depend on how quickly it is diagnosed and treated. Early intervention can help preserve kidney function and improve overall health outcomes for patients.
If left untreated or if treatment is delayed, patients may experience permanent kidney damage leading to chronic kidney disease or end-stage renal failure requiring dialysis or transplantation. Regular monitoring and follow-up care are essential for managing potential complications associated with this condition.
Can AHUS disease be inherited?
Atypical Hemolytic Uremic Syndrome (AHUS) can have a genetic component; many cases are linked to inherited mutations in genes responsible for regulating the complement system. Familial forms of AHUS have been documented.
This means that individuals with a family history of AHUS may be at increased risk for developing the condition themselves. However, it’s important to note that not all cases arise from familial history; some individuals may develop AHUS without any known genetic predisposition.
What role do environmental factors play in triggering AHUS disease?
Atypical Hemolytic Uremic Syndrome (AHUS), while primarily genetic in nature, can also be influenced by environmental factors that trigger its onset. Infections are significant triggers; particularly bacterial infections like E. coli have been linked to precipitating episodes of AHUS in susceptible individuals.
Pregnancy complications such as pre-eclampsia and certain medications may also act as environmental triggers for those genetically predisposed to develop AHUS. Understanding these triggers can help manage risks associated with this rare condition more effectively.
What is the prognosis for someone diagnosed with AHUS disease?
The prognosis for individuals diagnosed with Atypical Hemolytic Uremic Syndrome (AHUS) varies based on several factors including promptness of diagnosis and initiation of treatment. Early intervention generally leads to better outcomes; many individuals can recover significant kidney function.
If treated appropriately, patients often lead relatively normal lives post-diagnosis. Conversely, delayed treatment may result in severe complications like permanent kidney damage or failure requiring long-term management strategies such as dialysis or transplantation.
Is there ongoing research related to AHUS disease?
Yes, ongoing research into Atypical Hemolytic Uremic Syndrome (AHUS) aims to better understand its underlying mechanisms, improve diagnostic criteria, and develop more effective treatments. Studies focus on genetic factors influencing susceptibility as well as novel therapeutic approaches targeting complement system dysregulation.
This research seeks not only to enhance patient outcomes but also aims at increasing awareness about this rare condition among healthcare providers and patients alike. Continued advancements will likely contribute significantly to improving care strategies for those affected by AHUS.
Conclusion – What Is AHUS Disease?
Atypical Hemolytic Uremic Syndrome (AHUS) is a rare, potentially life-threatening condition that damages the blood vessels, leading to hemolysis, thrombocytopenia, and kidney dysfunction. It is caused by genetic mutations or overactivation of the complement system, and the disease can be triggered by infections or other factors. Early diagnosis and treatment with plasma exchange, complement inhibitors, or kidney transplant can improve outcomes and help prevent long-term complications.