Depression can begin subtly, with feelings of sadness or hopelessness, but over time, it can escalate into a serious condition that affects daily life.
The Early Stages of Depression
Depression often begins slowly, and its symptoms may be difficult to spot at first. It can start with feelings of sadness or emotional numbness, gradually evolving into persistent emotional and physical symptoms that disrupt normal life. For many people, the onset is subtle—perhaps you start feeling “down” more often, but it doesn’t seem like it’s something that could lead to full-blown depression. However, understanding how depression starts can help people recognize early signs and seek help before it escalates.
Common Early Signs of Depression
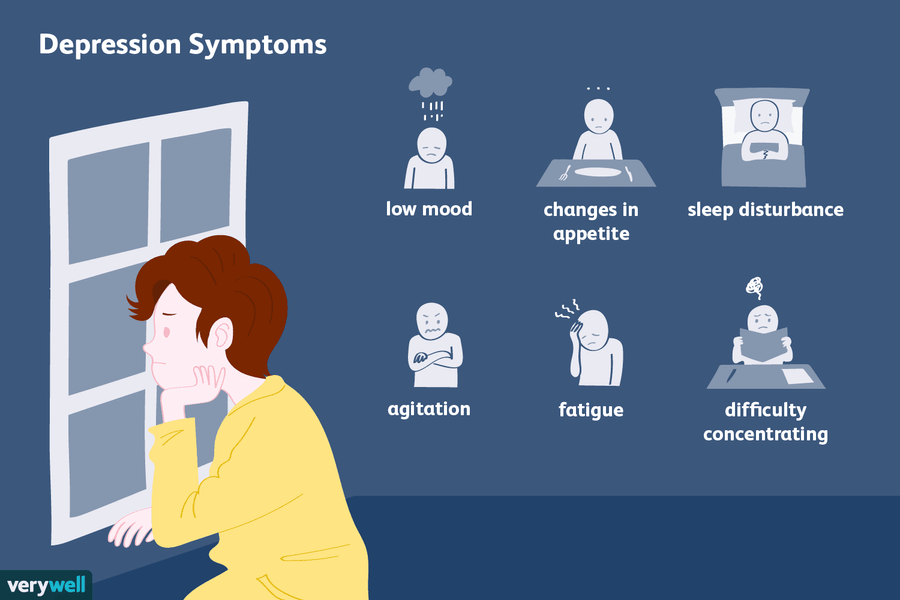
The early stages of depression can manifest in a variety of ways, and they might not all be obvious. Here are some of the initial signs that may signal the start of depression:
- Persistent sadness: A sense of sadness or emptiness that lingers even when there’s no clear reason for it.
- Loss of interest: Activities that once brought joy or excitement may no longer hold the same appeal.
- Fatigue and low energy: Even after a good night’s rest, you might feel physically drained or lethargic.
- Changes in sleep patterns: Sleeping too much or too little is common, as depression often disrupts sleep cycles.
- Changes in appetite: Some people may lose their appetite entirely, while others may begin to overeat, leading to weight fluctuations.
- Trouble concentrating: Focus and memory problems are often early indicators of depression, making it difficult to complete tasks.
Depression doesn’t always begin with dramatic symptoms. It can develop in a more insidious way, and by the time the signs are noticeable, the condition may already be taking hold.
What Causes Depression to Start?
The question of why depression starts is not easy to answer. Depression can be triggered by a variety of factors, and often it’s a combination of these that contributes to its onset. Let’s break down some of the most common causes:
1. Genetics and Family History
Genetics plays a significant role in the development of depression. If someone in your family has suffered from depression or other mental health conditions, you may have a higher likelihood of developing it yourself. Research suggests that individuals with a family history of depression are more likely to inherit a predisposition toward the disorder. However, genetics alone isn’t enough to trigger depression—it often requires additional environmental or psychological factors.
2. Chemical Imbalances in the Brain
The brain is responsible for regulating mood through complex interactions between neurotransmitters—chemicals that transmit signals between nerve cells. Imbalances in neurotransmitters like serotonin, dopamine, and norepinephrine can contribute to the development of depression. These imbalances might occur naturally, or they could be triggered by external factors like stress, trauma, or certain medical conditions.
3. Chronic Stress and Life Events
One of the most common triggers of depression is prolonged or intense stress. Major life events such as the loss of a loved one, divorce, job loss, or financial struggles can all be significant contributors to the onset of depression. The ongoing stress from these events can take a toll on the body and mind, leading to the depletion of emotional and mental resources.
Even less dramatic but ongoing stress—such as chronic work pressure or financial insecurity—can wear a person down over time, eventually contributing to depression.
4. Childhood Trauma and Abuse
Early-life trauma, including physical, emotional, or sexual abuse, can set the stage for depression later in life. These experiences can alter the way the brain responds to stress, potentially leading to chronic mental health issues. People who experience significant trauma may have a heightened stress response or develop negative thought patterns that contribute to depression. These past experiences can resurface in adulthood when life stressors become overwhelming.
5. Health Conditions and Chronic Illness
Chronic physical health conditions, such as heart disease, diabetes, or cancer, are often linked to depression. Living with a long-term illness can lead to physical pain, isolation, and feelings of hopelessness. Even autoimmune diseases, hormonal imbalances, and neurological disorders like Parkinson’s disease can impact mental health.
Medications used to treat chronic conditions can also have side effects that contribute to depressive symptoms. Some drugs, particularly corticosteroids, beta-blockers, and certain hormonal therapies, may interfere with brain chemistry and mood regulation.
6. Substance Abuse
Substance abuse, including alcohol and drug use, is often a contributing factor to depression. While drugs or alcohol may provide temporary relief from feelings of sadness or anxiety, long-term use can interfere with brain chemistry and make depression worse. Withdrawal from substances can also trigger or exacerbate depressive symptoms. For some people, depression begins as a result of self-medication, where they turn to substances to cope with emotional pain or trauma, eventually leading to a vicious cycle.
The Role of Negative Thinking and Cognitive Patterns
Cognitive theories of depression suggest that how we think about ourselves, the world, and the future plays a major role in the development and progression of depression. Negative thinking patterns can distort perception, leading to feelings of worthlessness, hopelessness, and despair.
Cognitive Triad: Self, World, Future
The cognitive triad, a term coined by psychologist Aaron Beck, refers to the three main areas that negative thoughts can impact in a person’s life:
- The self: A person may feel inadequate, incompetent, or unworthy.
- The world: They may view the world as an unforgiving, hostile place.
- The future: A bleak outlook on the future may make everything seem futile.
This negative thinking can spiral, reinforcing feelings of sadness and despair. Over time, this becomes a feedback loop that deepens depression.
Rumination and Overthinking
Rumination—repeatedly focusing on negative thoughts or events—can also contribute to depression. People who ruminate tend to replay upsetting situations in their minds, which can keep them stuck in a cycle of negative thinking. This often exacerbates feelings of helplessness, as the person feels unable to break free from their emotional distress.
How Depression Affects the Brain
When depression sets in, it can have a profound effect on the brain. Chronic stress, negative thinking, and chemical imbalances can alter brain function, making it harder to regulate emotions and handle stress. Certain brain areas, like the prefrontal cortex (responsible for decision-making and emotional regulation), can shrink in size during periods of prolonged depression. This may explain why it becomes increasingly difficult to "snap out of it" during depressive episodes.
Neuroplasticity and Depression
Neuroplasticity refers to the brain's ability to form new neural connections and adapt to changes. In individuals with depression, neuroplasticity can be impaired, leading to fewer healthy connections in areas of the brain that help manage mood and stress. Treatment for depression, including therapy, medication, and lifestyle changes, can promote neuroplasticity and help the brain heal.
The Gut-Brain Connection
Emerging research suggests that the gut and brain are closely linked. The gut microbiome, which consists of trillions of bacteria in the digestive system, can influence mood and mental health. Imbalances in the gut microbiome may contribute to depression, suggesting that improving gut health could have a positive impact on mental well-being.
Social and Environmental Factors
While individual factors are important, social and environmental circumstances also contribute to the development of depression. Support systems—such as family, friends, and community—can buffer against the effects of stress and reduce the risk of depression. On the other hand, social isolation and a lack of emotional support can make someone more vulnerable to mental health struggles.
The Impact of Social Media
In today's digital age, social media can also contribute to the onset of depression. Constant exposure to curated images of others' lives can lead to feelings of inadequacy, loneliness, and FOMO (fear of missing out). Comparisons with others, especially when experiencing personal struggles, can exacerbate feelings of sadness and low self-worth.
Economic and Societal Pressures
In societies where there is a strong focus on achievement, success, and productivity, people may feel immense pressure to meet societal standards. Economic downturns, job insecurity, or even societal inequalities can contribute to a sense of helplessness and frustration. For many, these factors can set the stage for depression to take root.
Conclusion: How Does Depression Start?
Depression is a complex condition that doesn’t have a single cause, but rather a combination of genetic, biological, psychological, and environmental factors. It often begins subtly, with small changes in mood or behavior that can easily be brushed off. However, if left unchecked, these early signs can evolve into a more serious and persistent problem.
Understanding how depression starts can help individuals recognize the signs early and seek appropriate help. Whether through therapy, medication, or lifestyle changes, there are ways to manage and treat depression. The earlier it’s identified, the easier it is to intervene and prevent the condition from worsening.