Bacterial vaginosis (BV) itself doesn’t directly cause infertility, but it can impact the chances of getting pregnant by disrupting the balance of bacteria in the vagina, potentially leading to complications.
What Is Bacterial Vaginosis (BV)?
Bacterial vaginosis is one of the most common vaginal infections, affecting millions of women worldwide. It occurs when the balance of bacteria in the vagina is disturbed, favoring harmful bacteria over the beneficial ones. This imbalance can lead to symptoms like unusual discharge, a fishy odor, and irritation.
However, BV isn’t always symptomatic. Many women with BV may not notice any symptoms at all. Despite this, even asymptomatic BV can affect reproductive health, raising concerns for women who are trying to conceive.
The question arises: Can BV stop you from getting pregnant? While BV itself isn’t classified as a sexually transmitted infection (STI), it shares some similarities with conditions that can interfere with fertility. Understanding the effects of BV on fertility, as well as how to treat and prevent it, can provide clarity for women trying to conceive.
How Does BV Impact Fertility?
Bacterial vaginosis doesn't directly cause infertility, but it can make it harder for women to get pregnant. There are several ways BV can affect the reproductive system:
1. Disrupting the Vaginal Environment
The vagina is home to a delicate ecosystem of bacteria, and maintaining a healthy balance is crucial for fertility. BV alters this environment, often lowering the pH of the vagina and creating conditions that are unfavorable for sperm survival. Sperm rely on a neutral pH to survive and travel toward the egg, and BV’s acidic environment can reduce their motility (movement), preventing them from reaching the egg.
This disruption can create challenges when trying to conceive, although BV itself may not cause complete infertility. The acidity brought on by BV makes the vaginal environment hostile, decreasing the chances of successful fertilization.
2. Increased Risk of Pelvic Inflammatory Disease (PID)
BV has been linked to an increased risk of pelvic inflammatory disease (PID), an infection of the reproductive organs. PID is a serious condition that can result from untreated BV, leading to scarring of the fallopian tubes and other parts of the reproductive system. Scar tissue can block the fallopian tubes, making it difficult for eggs to be fertilized or for embryos to travel to the uterus.
Even mild cases of PID can have long-term effects on fertility, particularly if both fallopian tubes become blocked. Women with PID are also at greater risk of ectopic pregnancy, a dangerous condition where the fertilized egg implants outside the uterus.
3. Preterm Birth and Miscarriage Risk
While the connection between BV and infertility is not fully established, BV is known to increase the risk of complications during pregnancy. Women with BV are more likely to experience preterm birth, low birth weight, and miscarriage. If a woman with BV conceives, the infection can trigger early labor or affect the development of the baby.
Although BV isn’t a direct cause of miscarriage or preterm birth, it is a risk factor. Therefore, treating BV before pregnancy may lower the chances of complications once conception occurs.
4. Increased Susceptibility to STIs
Women with BV are more vulnerable to other sexually transmitted infections (STIs), including chlamydia and gonorrhea, which can directly affect fertility. The presence of BV can make it easier for harmful bacteria and viruses to enter the reproductive system, heightening the risk of infections that can cause scarring, PID, or even infertility.
In some cases, women with BV may unknowingly contract an STI, which then leads to further complications with fertility. Regular STI screenings are important for women with BV to ensure that they are not harboring other infections that could impede their ability to conceive.
Can BV Be Treated?
The good news is that BV is treatable. Treatment generally involves antibiotics that target the bacteria responsible for the infection, such as metronidazole or clindamycin. Once the bacterial imbalance is corrected, the symptoms of BV typically resolve, and the vaginal environment is restored to a healthier state.
1. Antibiotics
Doctors usually prescribe oral antibiotics like metronidazole or clindamycin to treat BV. These antibiotics are effective in restoring the natural bacterial balance of the vagina, eliminating harmful bacteria and allowing the beneficial bacteria (like lactobacilli) to repopulate.
It is important to complete the full course of antibiotics, even if symptoms improve, to ensure that the infection is fully eradicated. In some cases, BV may recur, which can require further treatment.
2. Probiotics
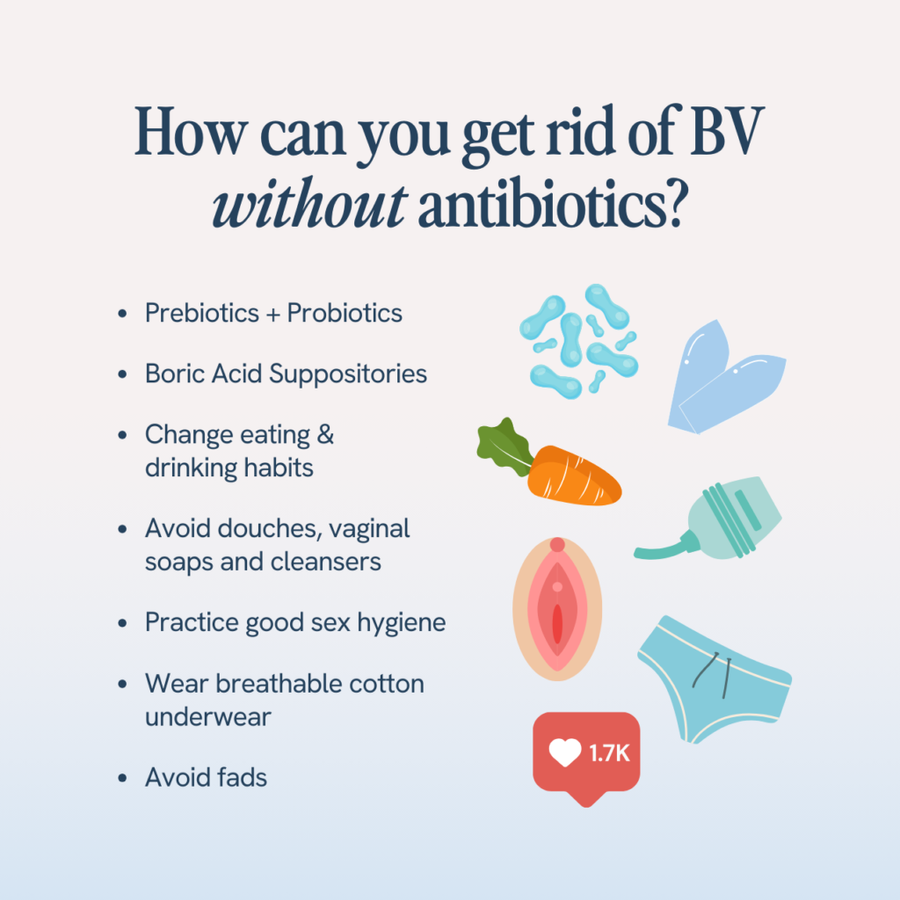
Probiotics, particularly those containing lactobacillus strains, may help restore a healthy balance of bacteria in the vagina. Some studies suggest that taking probiotics alongside antibiotics can help reduce the recurrence of BV. Additionally, probiotics can boost overall vaginal health, which may be beneficial when trying to conceive.
While there’s no definitive evidence that probiotics can cure BV on their own, they may help prevent further episodes and support the vaginal microbiome after treatment.
3. Home Remedies
Some women explore home remedies to treat BV, such as garlic, tea tree oil, and apple cider vinegar. However, while these remedies may help reduce symptoms, there’s limited scientific evidence to support their effectiveness in curing BV.
It's essential to consult with a healthcare provider before using home remedies, as they could potentially interfere with prescribed treatments or irritate the vagina.
Preventing BV and Supporting Fertility
If you are trying to conceive, preventing BV is an important step in maintaining reproductive health. There are several ways to reduce your risk of developing BV and to maintain a healthy vaginal environment:
1. Maintain Proper Hygiene
Keeping the vaginal area clean and dry is important for preventing infections, including BV. However, it’s important not to over-wash or use harsh soaps that can disrupt the natural balance of bacteria. A mild, unscented soap is often the best choice.
Avoid using douches, as they can irritate the vagina and wash away beneficial bacteria, increasing the risk of BV. Also, wearing breathable cotton underwear and avoiding tight clothing can help prevent the buildup of sweat and bacteria, which may contribute to infections.
2. Practice Safe Sex
Using condoms during sexual activity can help protect against STIs and reduce the risk of BV. While BV itself is not classified as an STI, it can be triggered by sexual activity, especially if there’s a change in sexual partners. Condoms can also help reduce the transmission of harmful bacteria between partners.
3. Limit Antibiotic Use
Overuse of antibiotics can disrupt the natural balance of bacteria in the body, including in the vagina. While antibiotics are necessary to treat infections like BV, they can also kill off the good bacteria that help protect against harmful bacteria. If you’ve recently taken antibiotics for another condition, consider supporting your vaginal health with probiotics or discussing preventive options with your doctor.
4. Regular Check-Ups and STI Screening
If you’re trying to conceive, regular gynecological check-ups and STI screenings are essential. This helps identify and treat any infections early before they can interfere with fertility. Women with BV or a history of recurrent BV should discuss their fertility goals with a healthcare provider, who can help create a treatment plan to minimize any risks.
Conclusion – Can BV Stop You From Getting Pregnant?
While bacterial vaginosis (BV) doesn't directly prevent pregnancy, it can make conception more difficult by disrupting the vaginal environment and increasing the risk of pelvic inflammatory disease (PID), which can block fallopian tubes and hinder fertility. Treating BV with antibiotics can restore balance and improve your chances of getting pregnant, but untreated or recurrent BV may contribute to complications such as miscarriage or preterm birth once you conceive.
Maintaining vaginal health through proper hygiene, safe sex practices, and regular check-ups can reduce the risk of BV and other infections, enhancing your fertility. If you're struggling with BV and trying to conceive, it's important to talk to your healthcare provider for a tailored plan to improve your reproductive health and increase your chances of a successful pregnancy.